SUZANNE O'CALLAGHAN
Suzanne O'Callaghan is HFA Policy Research and Education Manager
Plenary (Arosenius Lecture) – Towards novel treatment options in von Willebrand disease
Speaker ~ Peter Lenting, Director of Research, French National Institute of Health and Medical Research – INSERM, Paris, France
In the Arosenius Lecture medical plenary Peter Lenting explored some of the treatment issues for people with von Willebrand disease (VWD) and outlined some innovative treatments that are currently in the pipeline.
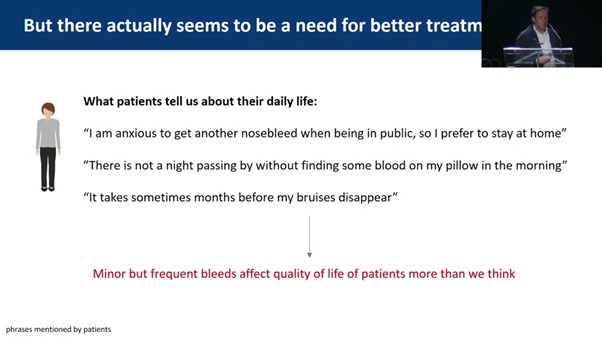
Although his VWD research is highly scientific, Peter Lenting consults his patients with VWD regularly to understand the impact of VWD and what outcomes they are seeking from treatment.
Clinicians would usually expect the biggest impact on quality of life to occur in severe forms of VWD. However, he has found there are also many issues for people with mild forms who experience frequent minor bleeds, especially women. Most patients with VWD have Type 1 (5-30% von Willebrand factor/VWF) and many are in the category now called VWFlow (30-50% VWF). They have frequent minor bleeds which do bother them and affect their quality of life.
As a result, he proposed the goals of VWD treatment should be:
For his patients, this included:
He outlined some current clinical trials and experimental studies and how they are contributing to these goals:
Emicizumab in Type 3 VWD
Nanobody therapy – currently experimental mice studies

Old Montreal
Photo: Shauna Adams
ROBYN SHOEMARK
Robyn Shoemark is Clinical Nurse Consultant Haemophilia/Haematology at the Kids Factor Zone, The Children’s Hospital at Westmead, Sydney, NSW.
Changing treatment, changes diagnosis
Chair ~ Kate Khair, Director of Research, Haemnet, London, UK
Non-factor therapy in persons with acquired hemophilia A and von Willebrand disease ~ Ming Lim, Assoc Prof, Division of Hematology and Hematologic Malignancies, University of Utah Health, Salt Lake City, USA
For patients with Type 3 VWD, standard treatment is factor VIII and von Willebrand factor (VWF). For patients who have developed an inhibitor to VWF or continue to bleed despite prophylaxis, standard treatment is plasma-derived FVIII/VWF or recombinant factor VIIa and there are few options for new treatments.
Ming Lim reported on a review of off-label use of emicizumab in 8 patients with Type 3 VWD, 3 with an inhibitor and 5 without an inhibitor with frequent bleeds. Results so far looked promising, providing haemostasis for these patients. Further studies need to be conducted to check and confirm the results.
Late-breaking Clinical Research
Chair: Glenn Pierce, Vice President Medical, World Federation of Hemophilia, USA
A phase 1 sequential pharmacokinetic (PK) evaluation of octocog alfa, rurioctocog alfa pegol, and efanesoctocog alfa in severe hemophilia A ~ Annemieke Willemze, Senior Clinical Research Director, Sanofi Genzyme, Amsterdam, Netherlands
Annemieke Willemze discussed the BIVV001 (efanesoctocog alfa) trial results in the Late Breaking Clinical Research session. In question time, there was a discussion about the use of BIVV001 for patients with Type 2N and Type 3 VWD. Results have been similar to people with haemophilia A, with a weekly treatment injection and an increase in the half-life of the treatment to an average of around 43 hours. This is good news for those patients with little to look forward to on the horizon of new treatment options.
Haemophilia Foundation Australia acknowledges the Traditional Owners and Custodians of Country throughout Australia, the land, waters and community where we walk, live, meet and work. We pay our respects to Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.
Sign up for the latest news, events and our free National Haemophilia magazine